Pharmacogenomic Testing Can Benefit Children and Families
Adverse drug reactions cause approximately 6% of all hospital admissions each year.

Pharmacogenomic testing is an essential tool for ensuring effective treatment with many medications and decreasing the risk of adverse events.
In Tuesday’s session, “Pharmacogenomic Testing in Children: Which Tests and What Comes After Testing?” Shannon Manzi, director of safety and quality in the pharmacy department at Boston Children’s Hospital, said the goal of pharmacogenomic testing is to reduce adverse drug reactions in patients.
“Hundreds of thousands of patients each year in the United States, let alone the rest of the world, are affected by adverse drug reactions,” she said. “And as you know, adverse drug reactions are those events that are relatively unexpected. There is no error involved. It was not the wrong patient or the wrong drug or the wrong dose given. These are (situations where) all the appropriate things were done and still the patient had a poor outcome.”
Adverse drug reactions cause approximately 6% of all hospital admissions each year, adding up to a billion dollars in costs for treatment. Manzi said if you add those together with medical errors, they are a leading cause of death in the United States.
“And that is quite a sobering statistic that we all need to keep in mind as we move forward and try to make medication use safer in our patients,” she said.
Manzi said pharmacogenomic testing can also be used as companion testing, which is sometimes required before initiating treatment, as well as a screening tool prior to the initiation of treatment. For medications with high toxicity profiles pharmacogenomic testing can be used in some cases to identify patients for whom those drugs might be beneficial and who may not have those high toxicity profiles.
There is a broad range of options available for pharmacogenomic testing, Manzi said. These include single nucleotide polymorphism panels and sequencing. There are also a number of phenotype classifications including ultrarapid, rapid, intermediate, normal, and poor metabolizers — depending on the gene expression and resultant enzyme production.
Manzi said pre-emptive pharmacogenomic testing is useful in a number of cases, particularly those where:
- The cost-savings generated by pre-emptive testing (e.g. preventing morbidity secondary to adverse drug reactions) is a major factor in offering testing.
- Medications are designed to only be effective with certain variant statuses (mutations) and, therefore, this is a key reason for offering pre-emptive testing.
Such testing has produced strong results at Boston Children’s Hospital. Manzi said approximately 92% of patients tested by one of the hospital’s panels have had an actionable result. She said this is extremely relevant to patient care.
“We’ve had some patients — about 36%— who had no significant finding for what they came for,” she said. “So they have a question, whether it is ‘what medication should I be on for depression’ or things along those lines. However, when we look at the entire panel, most of those patients — 89% — have come back with a significant, what we call incidental, pharmacogenomic result. Meaning that they didn’t come to us for pharmacogenomics but we can actually inform that now.”
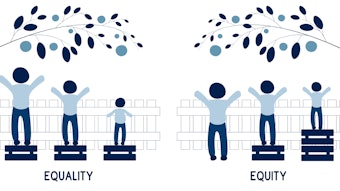
When considering whether pharmacogenomic testing is worth it, Manzi said there are a number of factors to weigh, including the number of people you need to treat, how much the test costs to run and interpret, whether it will be reimbursed, and the cost-savings that may be gained by pre-emptive testing. One factor they have stayed away from at Boston Children’s Hospital, however, is the ethnic factor.
“We originally had this question, and what we found is people don’t know what they are,” she said. “You hear from your grandparents and others that this is the history of our family. However, when we do testing, we find out that maybe that’s not exactly true. And so yes, we know that some variant statuses are more likely in certain ethnic populations, but we as an institution took the position that if we are offering it, we are offering it for everyone. That may not be the case for the way that others use this, but because of the population that we treat, it became evident that we were seeing a lot of rare variants in patients that we may not have expected based on the ethnic variation and so early on we made the decision that we were not doing it.”
Cyrine Haidar, clinical pharmacogenetics coordinator at St. Jude Children’s Research Hospital in Memphis, Tennessee, spoke about what comes after the testing is done and specifically how to deal with the familial implications of the testing and the results.
“There are certain pharmacogenes that are dominant in nature in genomic testing and so once we have a result for a patient we actually will know that there’s a likelihood that they got their results either from their mother or from their father and their siblings, (and that) may have some implications for the results that they have,” she said.
Haidar used malignant hyperthermia as an example. This, she said, is a genetically inherited, potentially fatal disorder that occurs due to an acceleration of metabolism in skeletal muscles. She said when they receive a test result showing this in a child, it means that one of the parents has that same high-risk result for malignant hyperthermia.
“The implications of that mean that if we know and if we see a patient who has a high-risk malignant hyperthermia result — meaning that they should not receive certain medications — we tell them that they should not receive these medications and that they are contra-indicated for them because of their risk of developing (the adverse effect),” she said. “We also could provide genetic counseling to the family of the patient to explain to them what the result means and what the implication of the positive test results are for the patient’s first-degree relatives — meaning their biological parents, their full biological siblings — and offer testing to the first-degree relatives.”
Whatever decision is made, Haidar said before any results are returned for any gene that has familial implications it is important to have a process set up and approved by your institution to answer certain questions, including:
- Should counseling of family members be performed?
- Should genotype testing of family members be offered?
- Should the institution follow-up with family members in the event of a high-risk result?
- Who will pay for the genotype testing?
“All of these are questions that should be established and you should have a process set up before you actually start returning these results because they will happen, and it is important to have a process at least discussed and preferably written before you have a patient who has a high-risk result,” she said.
Learn more in ASHP’s Statement on the Pharmacist’s Role in Clinical Pharmacogenomics.