New Research Brings Changes to the Medication-Use Process
MUP is critical to the relationship between pharmacists and patients.

The medication-use process (MUP) continues to evolve as it provides systems for the safe and effective use of medications.
The on-demand session “Practice Enhancing Interventions About the Medication-Use Process from 2020: Gems from AJHP,” features a dozen speakers taking a closer look at changes to the MUP highlighted in a 2020 AJHP article and what they will mean for pharmacy going forward.
Among the topics covered at the session will be a look at the management of an IV fluid shortage using electronic medical record alerts. Drug shortages pose a significant public health risk and can lead to denial or delays in critical therapy as well as the use of less safe or less effective medications.
Kruti Shah, clinical pharmacist specialist in drug information and drug policy development at Grady Health Systems in Atlanta, Georgia, will outline a study done at Grady Health during a shortage of IV fluids brought on by damage to an IV fluid manufacturer during Hurricane Maria in 2017.
Shah said the study found that the electronic medical alert system can help manage critical medications during a shortage situation.
“We did find that EMR alerts can be effective during drug shortages,” she said. “Conversion to alternate formulations can be a sustainable strategy as well. Based on clinical outcomes, we were able to eliminate the need for stocking multiple concentrations.”
Errors during transition of care are unfortunately common, with medication errors accounting for about half of those. But Sue Fosnight, clinical lead pharmacist and professor of pharmacy practice at Summa Health/NEOMED in Akron, Ohio, said pharmacists have a knowledge base that can impact the prevention of adverse events involving transition medication.
Fosnight will highlight an intervention developed at Summa Health that starts with a pharmacy technician then goes to a medication evaluation conducted by the pharmacist. From there, it involves the prescribers, looks at medication adherence barriers, affordability of medications, discharge reconciliation, and medication counseling, with flags for follow-up with the patient or caregiver if needed.
The results, Fosnight said, were a big improvement with a little more time investment from the pharmacist and the pharmacy technician.
“We found that 50 minutes of pharmacist time and 27 minutes of pharmacy technician time per patient were required for this pharmacy transition intervention,” she said. “That lead to an average of 9.56 medication changes per patient, and also contributed to a significantly decreased readmission rate and a significantly decreased length of stay.”
Tyler Vest, pharmacy manager of automation, medication distribution, and controlled substances for Duke University Hospital in Durham, North Carolina, said the MUP is critical to the relationship between pharmacists and patients.
“When I think about the medication-use process, I’m talking about the foundational system that provides safe and effective medication use,” he said. “What are the checks and balances that we have in place to care for our patients in the acute care setting or the ambulatory care setting throughout the health care system?”
Historically, the MUP has been seen as linear, with eight steps in the process from procurement and prescribing to administration and monitoring. But Vest said that process is changing.
“The medication use process does continue to transform and it continues to move forward with practice and is optimized by technology,” he said. “Some previous steps could become obsolete and there could be potentially new steps in the future as well. It’s kind of a continuing cycle of transformation.”
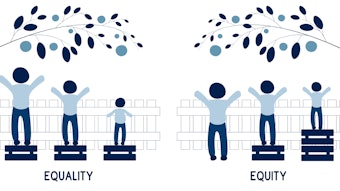
Vest said the process is now viewed more as a cyclical process, putting the patient right at the center, with some of the steps either removed entirely or combined with other steps.
“I think it’s just a different way to look at it and I think it’s just an alignment of who we are as a profession,” he said. “It is really putting the patient at the center of the things we do and making sure that we accurately, safely and reliably care for these patients.”
For the purposes of the session, Vest said the presentation focuses on four main steps: prescribing and transcribing, dispensing, administration, and monitoring.
“If we don’t have these processes set up correctly, if we aren’t doing the right things to care for these patients from a process standpoint then obviously that is going to have an impact on patient safety,” he said.
Other topics covered at the session include the effect of order entry alerts and modifications on doses of IV opioids dispensed during a national shortage, the impact of interoperability of smart infusion pumps and an electronic medical record on critical care, and the Rural VA Multi-Center Medication Reconciliation Quality Improvement Study.
Vest said this session is important for pharmacists looking to keep up with an ever-changing area of their operations.
“The MUP is continually evolving as new health care technologies are introduced and there is also literature being published that demonstrates new and better ways, innovative ways, and different ways to care for our patients,” he said.
Read Practice-enhancing publications about the medication-use process in 2020, published Nov. 13 in AJHP.